SYMPTOMS, SIGNS, CAUSES AND TREATMENT OF ECTOPIC PREGNANCY
The word ectopic is derived from the Greek word “Ektopos” meaning out of place. After fertilization which is the union of the egg and sperm, the fertilized egg moves to the womb and gets implanted. In ectopic pregnancy this does not happen instead, it is implanted outside the womb.
The prevalence is estimated at 1 in 40 pregnancies or 25 cases per 1000 pregnancies according to the United States centre for disease control and prevention. The incidence has been rising due to improvement in early diagnosis, resulting in the discovery of those that would have resolved naturally without treatment. However, some authorities might argue that the increased incidence is as a result of previous pelvic infection. However, the death rate is falling due to early diagnosis and treatment.
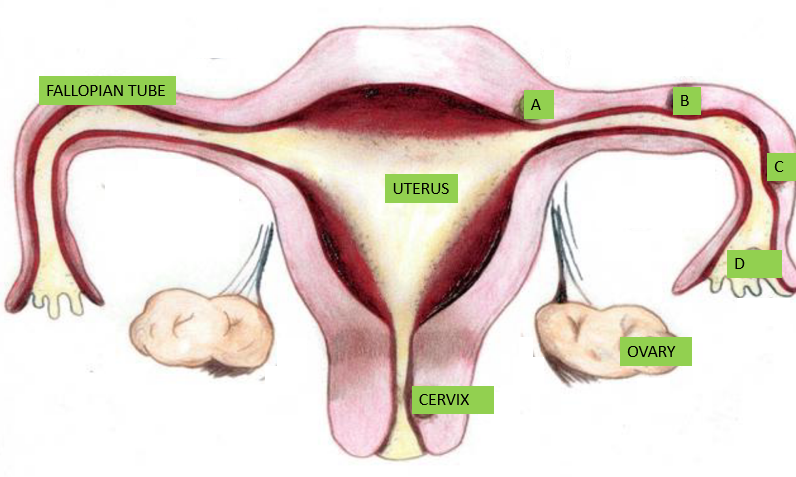
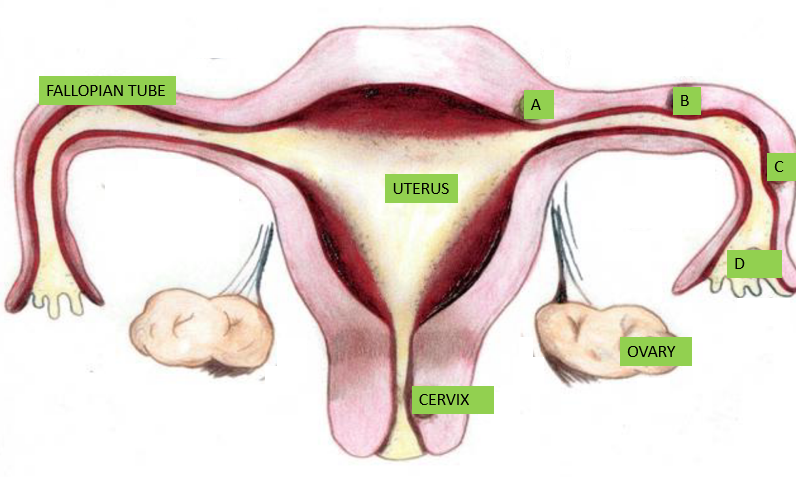
Ectopic pregnancy commonly occurs in the fallopian tubes, other areas in descending order of occurrence includes; the abdomen, ovary and cervix though they rarely occur here. Rarely a normal pregnancy can co-exist with an ectopic pregnancy; this is called heterotopic pregnancy. It is one of the common causes of severe bleeding and death in early pregnancy hence the need for an early scan to locate the pregnancy. The exact cause is not known but there are risk factors that predispose to having ectopic pregnancy.
RISK FACTORS FOR ECTOPIC PREGNANCY
Some women who had ectopic pregnancy had no risk factors however, anything that stops or delays the movement of the fertilised egg to the womb where it normally implants can result in ectopic pregnancy.
- Non-treatment or poorly treated pelvic inflammatory disease (PID) which is sexually transmitted.
- Adhesions from pelvic surgeries.
- Endometriosis.
- Previous surgery on the fallopian tube.
- When the tubes have been tied and it fails.
- Smoking.
- Some hormonal contraceptives when they fail.
- Women with inability to conceive who then use assisted reproductive technology, example in-vitro fertilization (IVF) or use of clomiphene. (Do not abuse clomiphene because you want twins)
- Previous history of ectopic pregnancy has a 10 to 20% chance of recurrence.
- Age ≥ 35 years is associated with a higher rate of ectopic pregnancy.
- A scared womb.
- Fibroid.
SYMPTOMS AND SIGNS OF ECTOPIC PREGNANCY
There are three common symptoms 50% of women with ectopic pregnancies might have such as;
- History of Loss of menses.
- Abdominal pain.
- Sudden vaginal bleeding.
Some symptoms might be like those of early pregnancy such as;
- Nausea
- Vomiting
- Tiredness
Others symptoms may be;
- Dizziness
- Weakness
- Sudden collapse/fainting
- There may be a swelling at the site where the pain is maximum
- Sudden recent pain during sex
- Shoulder pain
- Diarrhoea
- Pain while defecating
- Fever.
You do not have to notice all the above symptoms or all the major symptoms before you go to the hospital.
At the emergency room, the doctor will ask a few questions to establish the symptoms of ectopic pregnancy and carry out examination to elicit signs that will help make the diagnosis. These signs will give an idea whether it has ruptured or not and the severity of the situation. When the ectopic pregnancy ruptures, the blood accumulate in the abdomen and cause irritation resulting in the following signs;
-Fast breathing.
-Low blood pressure and high pulse.
-A painful abdomen when pressure is applied on it and when the pressure is quickly remove.
-A very rigid abdomen.
-Pain when the cervix is moved.
Ectopic pregnancy is “a black cat masquerading in the dark” because other disease state mimics it. A high index of suspicion is required as it can be mistaken for an appendicitis, PID, urinary tract infection,ovarian torsion or cyst.
TREATMENT OF ECTOPIC PREGNANCY
The treatment for ectopic pregnancy depends on when it was diagnosed and the clinical state of the woman. When discovered incidentally early in pregnancy during routine scan the treatment might be expectant or medical treatment for ectopic pregnancies that have not ruptured.
When a woman meets the criteria for expectant treatment, which is assessed from the result of the pregnancy hormone called β-Chorionic gonadotrophin (β-HCG), other blood tests, ultrasound scan, her general clinical state (which should be stable) and her understanding of her condition, then, an expectant treatment can be undertaken. She will be adequately counselled by her healthcare provider on the possible chances of the ectopic pregnancy rupturing and the need to come for follow up visits as scheduled to check for blood levels of the pregnancy hormone (β-HCG) which is expected to be falling. Medications are usually not given; the pregnancy is observed for spontaneous resolution.
When a woman meets the criteria for medical treatment, she will be advised by her healthcare provider to avoid alcohol, vitamins containing folic acid, sexual intercourse and nonsteroidal anti-inflammatory drugs(NSAIDS) example diclofenac during the course of her medical treatment. She will be treated using methotrexate which is the common medication used, other medications include; potassium chloride or hypertonic saline. She will be counselled of the possibility of the ectopic pregnancy rupturing and the need to seek immediate care if she feels strange symptoms. At follow-up visits, the blood level of β-HCG would be checked and it is expected to be decreasing.
Furthermore, treatment could be surgical which could be conservative or non-conservative surgery. The decision to do either one will depend on if the fallopian tube has ruptured or not, the desire for future fertility and the state of the other tube as seen during the surgery. This could either be open surgery or minimally invasive surgery such as laparoscopy. Laparoscopy is the goal standard as it can be used both for diagnosis and treatment. It also has the advantage of less pain after surgery and short hospital stay. The demerit is that, is it expensive and requires a highly skilled operator. The conservative surgeries where the fallopian tube affected is preserved are for unruptured ectopic pregnancies but they constitute risk factors for a repeat ectopic pregnancy. The non-conservative surgeries are for ruptured ectopic pregnancy where the affected tube is removed.
The duration of stay in the hospital depends on the nature of the surgery or presence of any complication arising from blood loss or the surgery. Most patients treated with laparoscopy are discharged within 24 hours. Thereafter, the blood level of the β-HCG will continue to be monitored weekly until it becomes normal especially with some conservative surgeries. Ectopic pregnancy is a gynaecological emergency; the outcome is best when diagnosed early. Once a home or hospital pregnancy test turns out positive, the next thing to do is to confirm the location of the pregnancy.
I hope this article was helpful, you can leave a question or comment and I will surely get back to you.

-
27 July 2020 @ 11:25 PM
–
-
27 July 2020 @ 11:30 PM
–
A TRUE SUCCESS STORY OF A MISSING TWIN - ujahealth
21 June 2022 @ 2:32 AM
[…] pregnancy called “heterotopic pregnancy”. This is a huge success story as far as ectopic pregnancy is concerned. That’s why an early scan is very important not only to know where the pregnancy […]
SELF HOME PREGNANCY TEST - ujahealth
21 June 2022 @ 3:03 AM
[…] care provider of the danger at hand and the various treatment options available to you to avert it. ECTOPIC PREGNANCY IS A GYNECOLOGICAL […]